Urogenital Probiotics for Women
Overview
Probiotics are useful for more than just gastrointestinal health. In fact, there are specific probiotic products that can help prevent and treat female urogenital conditions like bacterial vaginosis, vulvovaginal candidiasis, urinary tract infections and related complications of all three.
This should not come as a huge surprise. The amount of good research being conducted on gastrointestinal probiotics continues to increase every year. And although the vaginal tract is not internally connected to the alimentary canal the two are intimately related. Bacteria that pass through the digestive system can ascend via the perineum to the vagina. So it's almost a no-brainer to expect what promotes gastrointestinal health to have relevance for urogenital health. However, they are not the same. Even though the intestinal microbiota has similarities to the vaginal microbiota, simply taking care of the intestinal microbiota may not be enough to ensure urogenital health.
Vaginal Microbiota: What Is It?
The microbiota typically found in the vaginal consists of large numbers of lactobacilli (gram-positive rods) and small numbers of gram-negative rods and gram-positive coccobacilli. A milliliter of vaginal fluid contains, on average, around 100 million microorganisms from 5-10 species, 95% of which are from the genus Lactobacillus (Anukam, 2006).
The bacteria that live in the vagina are substantially similar in all women around the globe. Â This is indicative of a relationship that was established long ago and which has remained robust over time. From an evolutionary perspective, such a trend suggests an adaptive advantage for both bacteria and humans. But why? A simple answer is that certain bacteria get a warm, moist place to live and in exchange, protect the vagina and help inhibit the growth of pathogens.
Health From The Few
It has been a long held belief that lactobacilli, in bulk, promote vaginal health by helping to maintain an acidic pH in the vagina. The logic seems sound: increased vaginal pH and decreased numbers of lactobacilli are symptomatic of various infections ergo lactic acid producing lactobacilli likely prevent infection by maintaining a low vaginal pH. This rationale has led to recommending the consumption of yogurt with the expectation that the lactobacilli, particularly L. acidophilus, and other active cultures should promote vaginal health.
Poking under the hood of this theory led to some interesting observations. Researchers discovered that the interaction of microorganisms in the vagina is more complex than simple pH modulation. The watershed: finding healthy women who appeared to lack colonization by lactobacilli. If large numbers of lactobacilli were necessary to regulate vaginal pH in most women, how could these exceptions be reconciled? It turns out that these women did not lack lactobacilli, they were merely present as an extremely small minority. But the fact that they existed in such small quantities suggested that there were mechanisms of vaginal health more potent than simple lactic acid production.
Lactic acid production was not found to be unimportant; rather something akin to a urogenital 90:10 rule had been identified. Most lactobacillus strains produce lactic acid, but only some strains produce bacteriocins and other specific regulating factors that inhibit the adhesion, colonization, growth and survival of undesirable species. Such specific factors can have prominent effects even at very low concentrations. And the strains that produce them can be present in miniscule amounts, but still have a large effect on urogenital health. Those healthy women with very few lactobacilli helped elucidate this.
Bacterial Vaginosis: Under the Radar
Bacterial vaginosis (BV) is the most common vaginal infection and is believed to be a problem for roughly 10-29% of the female population at any given time (Allsworth, 2007; Reid and Heinemenn, 1998). It is important to be aware that lactobacilli levels tend to track estrogen levels. This means that even for women that feel healthy, there can be an increased risk of infection when estrogen levels are low, like at the beginning and end of the menstrual cycle, or after undergoing menopause. BV is estimated to burden the health care system to the tune of more than 4 million office visits per year in the U.S. alone (Van Kessel, 2003). Yet despite these numbers, it is believed that many cases of BV still go untreated or mistreated.
BV can be one problem that arises when the vaginal microbiota becomes unbalanced. BV is characterized by a shift in the vaginal microbiota from predominantly commensal microorganisms like lactobacilli, to others such as species in the genera Gardnerella, Atopobium and Prevotella. Some of these organisms produce amines that raise the pH in the vagina and cause a fishy smell. Clinically, the Amsel criteria or Nugent scoring is used to diagnose BV.
The symptoms of BV are somewhat similar to those of a yeast infection, of which more women are aware. Since these symptoms tend to be a sensitive topic and because over-the-counter anti-fungal treatments are readily available, many women attempt to treat BV with anti-yeast remedies. Unfortunately, anti-fungal treatments do not help treat BV and can even make it worse.
Ounce of Prevention
Although not internally connected, bacteria that pass through the alimentary canal can ascend to the vagina over the short external distance of the perineum. This is entirely normal and not an issue of poor hygiene. In fact, this is the typical route to the vagina for most inhabitants. Knowing this, it stands to reason that a healthy urogenital environment can begin with a healthy digestive tract.
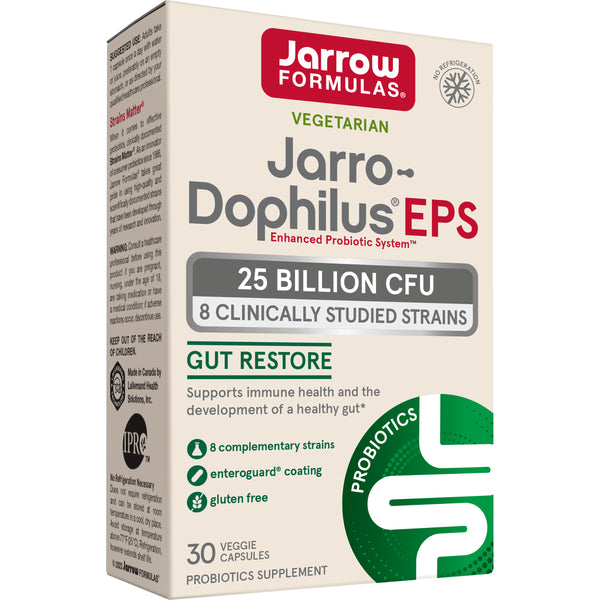
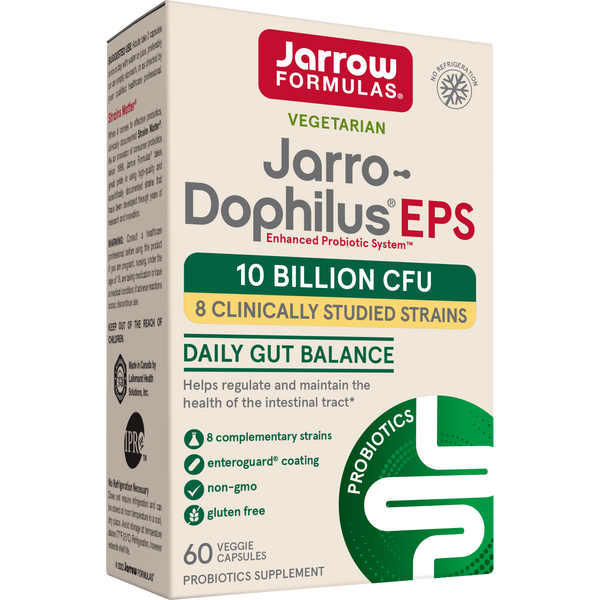
Beneficial intestinal microbiota, are more apt to flourish when exposed to a diet high in fiber (especially prebiotic fibers) and low in simple sugars and refined carbohydrates. Pathogenic bacteria tend to proliferate at a greater rate than probiotic bacteria when exposed to these hallmarks of a diet high in processed foods. The healthier the intestinal microbiota is, the lower the concentration of disruptive organisms that pass from the digestive tract to the vagina. Eating yogurt with live active cultures may help, although the clinical evidence to support this is somewhat equivocal. Digestive health may be better served by taking a probiotic product or supplement that contains multiple strains which are clinically documented to support health.
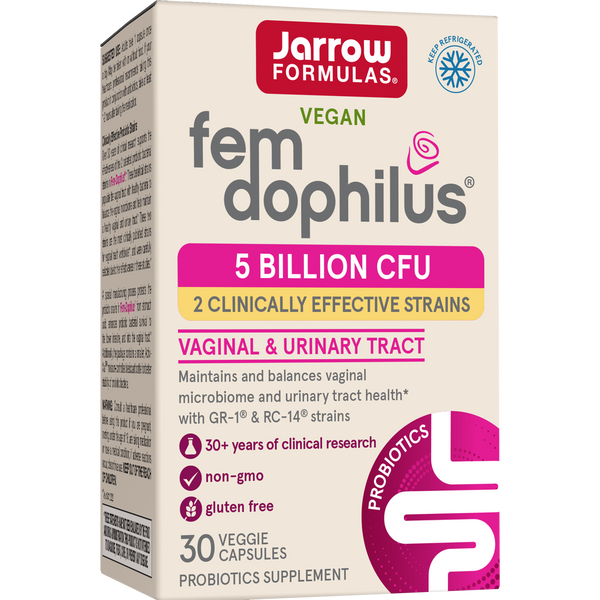
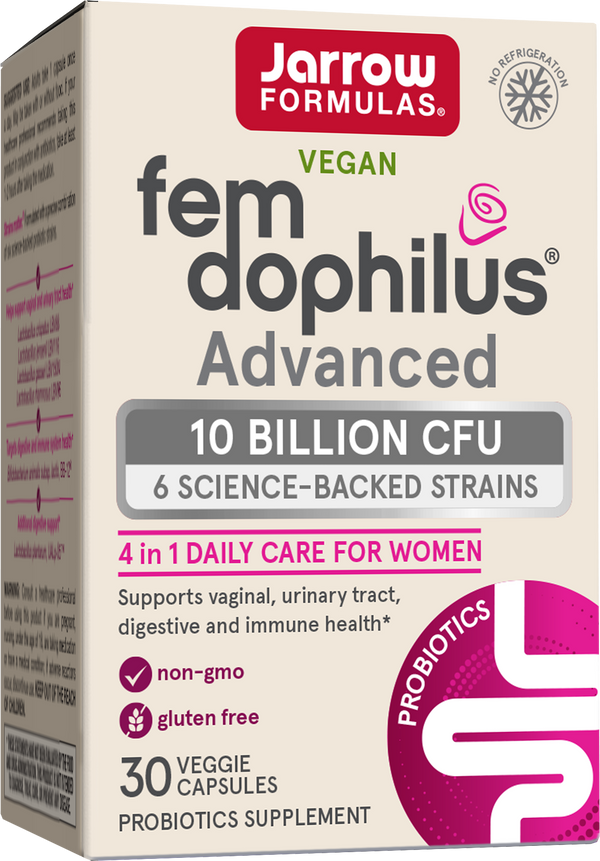
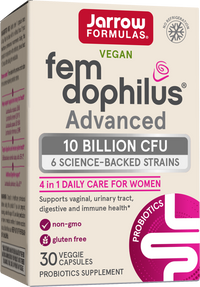
Women can also act preventatively against BV with probiotic products that have been specifically evaluated for vaginal health and found to promote healthy vaginal microbiota. An ideal choice would be a strain that was originally isolated from a healthy woman and is well characterized to act against vaginal offenders. There are very few products on the market made with probiotic strains that actually meet this standard. Two strains that do are Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Used together, L. rhamnosus GR-1 and L. reuteri RC-14 have been shown to promote healthy vaginal microbiota which is important in helping prevent BV (see Research Review).
BV Treatment & Probiotics
Standard treatment for bacterial vaginosis involves antibiotic therapy, either orally administered or locally applied. The oral route typically involves daily ingestion of metronidazole or clindamycin for one week. Locally, a metronidazole gel or 2% clindamycin cream may also be prescribed for a similar duration. Some reports find that using clindamycin leads to a greater rate of recurrence than metronidazole. In addition, local use of clindamycin is contraindicated for pregnant women because of a possible connection to birth defects. Regardless of which antibiotic option is used, statistics show that roughly 30% of BV infections recur within one month and approximately 80% within 9 months.
Increasing numbers of physicians are recommending that their patients follow a regimen of antibiotics with a course of probiotics for gastrointestinal health, to bolster beneficial bacteria that have been killed off. The same advice applies to urogenital probiotics. The vaginal microbiota is just as susceptible to broad-spectrum antibiotics as the intestinal microbiota. And although there is not any solid evidence to suggest probiotics alone are effective as treatment for an existing infection, probiotic supplementation can provide dividends before, during and after antibiotic treatment. As summarized in the Research Review, some probiotic strains can even improve the effectiveness of BV treatment with antibiotics.
Secondary Effects of BV: Preterm Labor & STI Acquisition Risk
Awareness about BV is particularly important because it can cause health concerns that are more serious than the immediate symptoms that women tend to notice: irritation, decreased well-being, and diminished sexual health. BV can lead to local inflammation, increased susceptibility to sexually transmitted infections and a heightened risk of preterm labor in pregnant women.
In the U.S. 7-10% of all babies are delivered preterm, while it is estimated that women threatening preterm labor cost the U.S. healthcare system $360 M annually. The total number of preterm deliveries has actually risen in the U.S. over the past ten years, as well. This is a bit troubling, although not incredible. Pregnant women are increasingly being given antibiotics to fend off group B streptococci found in their vaginas and also as a precautionary measure when the amniotic sac ruptures prematurely. Increased antibiotic use on average means more frequent assaults on the vaginal microbiota of pregnant women leading to a greater overall risk of BV.
Despite medical science not having a good grasp of what causes preterm labor, it has been known for some time that there is a correlation between the incidence of BV in an expectant mother and preterm delivery (Chaim, 1997; Hillier, 1992; Purwar, 2001). As mentioned above, antibiotics used to treat BV or other conditions can cause complications during pregnancy and disrupt the microbiota of the mother. Disruption of the microbiota is a concern because transmission of endogenous bacteria from mother to newborn occurs during birth and shortly thereafter, helping to establish the newborns own microbiota and immune system. Because of this association, the use of antibiotics to treat pregnant women has drawbacks. It has previously been hypothesized that probiotic therapy could help eliminate the conditions that cause preterm labor and hence avoid preterm labor itself (Reid, AJOG, 2003). Some preliminary research suggests that urogenital probiotics can help diminish the risk of preterm labor (see Research Review).
Sexually Transmitted Infections
The incidence of BV has also been associated with a greater occurrence of sexually transmitted infections like HIV (Anukam, Sex Transm Dis, 2006; Sewankambo, 1997), cytomegalovirus (Ross, 2005), chlamydia (Nilsson, 1997; Joesoef, 1996), gonorrhea (Joesoef, 1996) and pelvic inflammatory disease (Brotman, 2007). For the most part, the connection between BV and increased risk of STI remains a question of causation or correlation. Research continues into understanding the mechanisms of BV and STI acquisition and the connection between the two.
Vulvovaginal Candidiasis: Bacteria v. Yeast
More commonly known as yeast vaginitis or colloquially as a "yeast infection", about 75% of women have an occurrence of vulvovaginal candidiasis (VVC) in their lifetime. Recurring problems of the bacterial microbiota, like BV, can make VVC more common, recurrences more likely, and outbreaks more difficult to treat. Standard prescription treatment includes oral antimycotics like fluconazole used daily for two weeks. Local antifungal creams and pessaries are common by prescription or available over-the-counter. Topical treatments have a tendency to eliminate superficial parts without reaching embedded parts of the causative organisms. VVC treatment can also inhibit the growth of endogenous lactobacilli present in the vagina.
VVC results from an over proliferation of Candida species (Candida albicans accounts for 85-90% of infections), a group of organisms that are commonly present in the vagina at low levels. A Candida bloom often causes increased inflammation of the vaginal mucosa and can lead to vaginal discharge and irritation. VVC is often characterized by a thick, whitish and non-uniform discharge that does not typically possess a fishy odor. Irritation during sexual intercourse and itchiness/inflammation of the vagina and surrounding area is common. Clinically, microscopic examination of a vaginal smear after treatment with 10% KOH can allow visualization of Candida hyphae.
A healthy urogenital microbiota decreases the risk of VVC. As discussed previously, there are some steps women can take to promote a healthy urogenital microbiota including taking targeted probiotic strains. Prophylactic probiotic use is one way to support a healthy microbiota and inhibit the uncontrolled growth of Candida yeasts (Reid, 2003, FEMS). No probiotic studies to date have shown efficacy in treating an existing infection alone, but there have been some preliminary results that suggest standard antifungal treatment in combination with a L. rhamnosus GR-1/L. reuteri RC-14 probiotic resulted in significantly less symptoms of yeast infection as compared to standard treatment alone (see Research Review).
Bacteria Out of Place
It is estimated that 25-30% of women between the ages of 20 and 40 have had at least one urinary tract infection (UTI). In 85% of cases, the bacteria responsible for a UTI originate in one's own intestine or vagina. Recurrent infections are common. Nearly 20% of women who have one UTI will have another.
UTI can be another casualty of an unhealthy urogenital microbiota. A UTI is a bacterial infection of the urinary system including the kidneys, ureter, bladder, and urethra. Urinary tract infections are one of the most common causes of doctor visits for women. UTI usually presents with a frequent need to urinate along with a burning sensation upon urination. Urine can appear cloudy or off-smelling. Pain, tenderness and pressure near the bladder are also common. Typical clinical evaluation involves urinanalysis to detect nitrites, leukocytes and leukocyte esterase.
Standard treatment for UTI involves a regimen of oral antibiotics for 7 days, typically trimethoprim or co-trimoxazole. Recurrences may be an indication of cystitis, where bacteria invade the umbrella cells making innate immune factors and antibiotics less effective. A healthy urogenital microbiota decreases the risk of urinary tract infections. A urogenital probiotic can be used while undergoing treatment with antibiotics to hasten recovery, to decrease side effects, and to begin establishing beneficial vaginal microbiota that will help guard against recurrence.
Overall, the message that needs to be reiterated to patients is that urogenital health is not about the absence of bacteria, but rather the proper balance. Probiotic strains that have been clinically tested for their efficacy in supporting urogenital health are an excellent option for promoting a balanced urogenital microbiota and preventing infection. Prevention deserves serious consideration as the treatment options for vaginal infections can sometimes be of limited efficacy, especially for recurring infections. Urogenital probiotic strains can also be a helpful adjuvant to standard treatment in many cases, helping mitigate side effects and in some cases bolstering treatment efficacy. Urogenital problems plague many women and cause much concern; women are often very relieved to learn that there is more they could be doing. Tell them.
Urogenital Probiotics: A Research Review
Effects on Urogenital Microbiota
Forty-two clinically healthy women were randomized into three treatment groups and one control group. The treatment groups received various oral dosage regimens of a L. rhamnosus GR-1/L. reuteri RC-14 (GR-1/RC-14) probiotic supplement and the control group received L. rhamnosus GG every day for twenty-eight days. All three treatment groups saw a significant increase in healthy vaginal microbiota, while the control group remained the same. The twice-daily treatment group accrued the most beneficial effects with 90% of patients retaining a normal vaginal microbiota two weeks after treatment. The study suggests that a daily dosage of about 1 billion (109) live GR-1/RC-14 organisms is adequate as a preventative regimen (Reid, 2001, FEMS).
Lactobacilli, Yeasts & Coliforms
Sixty-four clinically healthy women were randomized into two groups. The treatment group received a once-daily oral GR-1/RC-14 supplement while the control group received a capsule containing calcium carbonate for sixty days. Microscopy analysis on day 28 found that the treatment group had an almost 10-fold increase in lactobacilli over baseline and a significantly smaller increase of yeast and coliforms compared to placebo (Fig. 1). In contrast, the placebo group showed decreased counts of lactobacilli and larger increases in yeast and coliforms (Reid, 2003, FEMS).

Fig. 1: Average (Log) Difference in Microbiota Populations after 1 Months Daily Use
Bacterial Vaginosis Prevention
In the previous study, Nugent scoring by a blinded technician was used to assess the prevention of BV. The GR-1/RC-14 group fared much better than did the control group. Of those possessing a healthy vaginal microbiota at the outset, 24% (6/25) of the women in the placebo group developed BV by day thirty-five of the study compared to 0% (0/23) in the treatment group (Reid, 2003, FEMS).
BV Treatment in Combination with Antibiotics
Following BV infection, combination treatment using GR-1/RC-14 (1 capsule, 10 billion CFUs, b.i.d.) with metronidazole (500 mg, oral, b.i.d.) more than doubled (88%) the effectiveness of metronidazole alone (40%) in returning the vaginal microbiota to a healthy state (Fig. 2). Of the remaining 12% of patients in the treatment group whose microbiota were not judged to be healthy at follow-up, all were found to have an intermediate status with zero cases of BV (Anukam, 2006).

Fig 2: Effectiveness of Metronidazole + GR-1/ RC-14 Probiotic in Treatment of BV
Preterm Labor
Thirty pregnant women, who were diagnosed with BV and identified clinically as being at high risk of preterm delivery, were randomized into two groups. The treatment group was given a once-daily oral GR-1/RC-14 capsule for 15 days. The control group was not given any type of lactobacilli, but was monitored according to the clinical standard. Upon follow-up one month later, the treatment group showed much better vaginal health with decreased indicators of BV. But more importantly, 100% of the mothers in the treatment group, as opposed to 67% of the control group, delivered at term. No adverse events were reported (Dobrokhotova, 2007).
Vulvovaginal Candidiasis
Sixty-eight women who were positive for VVC were randomized into two groups and blinded. The treatment group received fluconazole (150 mg) plus 2 gelatin capsules of GR-1/RC-14 (10 billion organisms) once-daily for 28 days. The control group received fluconazole (150 mg) plus a placebo at the same schedule. After 28 days, the treatment group showed more than a three-fold decrease in both yeast levels and vaginal discharge compared to the control group (Martinez, 2009).
Urinary Tract Infections
One study sought to compare the recurrence rate of UTI in women treated with either standard 3-day antibiotic therapy alone or along with a GR-1 combination probiotic. First, either norfloxacin or co-trimoxazole was prescribed to the 41 women in this study. The norfloxacin group had a recurrence rate of 29% while the co-trimoxazole group recurred at a rate of 41%. Afterward all women were then randomized into two groups and administered a GR-1 combination product or sterilized skim milk as a pessary. These vaginal suppositories were given twice a week for two weeks, with two additional instillations at 4 weeks and 8 weeks. The GR-1 group had a recurrence rate of 21% over the ensuing 6 months, while the skim milk group showed a 47% incidence of recurrence (Reid, 1992).
In another randomized, double-blind study, recurrence rates of UTI were again the primary endpoint. A weekly GR-1 combination probiotic (10 billion CFUs) was given as a pessary for one year. This resulted in a decreased UTI occurrence rate from 6 per year, for these patients in the year prior to the study, to only 1.6 per year during the study (Reid, 1995).
References
- Allsworth JE, Peipert JF. (2007) Prevalence of bacterial vaginosis: 2001-2004 national health and nutrition examination survey data. Obstetrics and Gynecology 109: 114-120.
- Anukam KC et al. (2006) Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes and Infection, 8: 1450-1454.
- Anukam KC et al. (2006) Lactobacillus vaginal microbiota of women attending a reproductive health care service in Benin city, Nigeria. Sex Transm Dis. Jan;33(1):59-62.
- Brotman RM et al. (2007) Findings associated with recurrence of bacterial vaginosis among adolescents attending sexually transmitted diseases clinics. J Pediatr Adolesc Gynecol. Aug;20(4):225-31.
- Chaim et al. (1997) The relationship between bacterial vaginosis and preterm birth. A review. Arch Gynecol Obstet. 259:51-58.
- Dobrokhotova YE and Sci M. (2007) Modern approaches to the treatment of vaginal dysbiosis in pregnant of high risk groups. All-Russian Scientific Forum: Mother and Baby. October 2, 2007.
- Hillier SL et al. (1992) The relationship of hydrogen peroxide-producing lactobacilli to bacterial vaginosis and genital microflora in pregnant women. Obstet Gynecol. Mar;79(3):369-73.
- Joesoef MR et al. (1996) Coinfection with chlamydia and gonorrhoea among pregnant women and bacterial vaginosis. Int J STD AIDS. Jan-Feb;7(1):61-4.
- Martinez RC et al. (2009). Improved treatment of vulvovaginal candidiasis with fluconazole plus probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Lett Appl Microbiol Mar;48(3):269-74.
- Nilsson U et al. (1997)Â Sexual behavior risk factors associated with bacterial vaginosis and Chlamydia trachomatis infection. Sex Transm Dis. May;24(5):241-6.
- Purwar M, et al. (2001) Bacterial vaginosis in early pregnancy and adverse pregnancy outcome. J Obstet Gynaecol Res. Aug;27(4):175-81.
- Reid G, et al. (2003) Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunology and Medical Microbiology 35: 131-134.
- Reid G and Bocking A. (2003) The potential for probiotics to prevent bacterial vaginosis and preterm labor. Am J Obstet Gynecol. 189:1202-8.
- Reid G, et al. (2001) Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora. FEMS Immunology and Medical Microbiology 32: 37-41.
- Reid G, Heinemann C: The role of the microflora in bacterial vaginosis. In: Medical Importance of the Normal Microflora (Tannock GW, ed.), Kluwer, London, 1998, pp. 477-486.
- Reid G, Bruce AW, Taylor M. (1995) Instillation of Lactobacillus and stimulation of indigenous organisms to prevent recurrence of urinary tract infections. Microecology Therapy;23:32-45.
- Reid G et al. (1992) Influence of three-day antimicrobial therapy and Lactobacillus vaginal suppositories on recurrence of urinary tract infections. Clin Ther; 14 (1): 11-16.
- Ross SA, et al. (2005) Association between genital tract cytomegalovirus infection and bacterial vaginosis. J Infect Dis. Nov 15;192(10):1727-30.
- Sewankambo NÂ et al. (1997) HIV-1 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet 350:546-550.
- Van Kessel K, Assefi N, Marrazzo J, Eckert L (2003) Common complementary and alternative therapies for yeast vaginitis and bacterial vaginosis: a systematic review. Obstet Gynecol Surv 58:351-358.
Article by Brad J. Douglass, Ph.D. Brad is a Technical Specialist for Jarrow Formulas. He obtained his Ph.D from USC in Organic Chemistry where his research efforts concentrated on drug discovery. He was also a postdoctoral fellow at USC where he investigated novel blood-brain barrier transport methods for use in drug delivery to the brain.